Use our SOAP note template as a starting point to customize yours to fit your business.
SOAP Note Template
Make work flow with Connecteam’s digital forms & checklists
- Easily create digital forms and checklists for any task your team needs to complete on the job
- Boost accountability by having employees add a signature, image, or location stamp
- Save time by choosing from a variety of ready-made templates
- Instantly receive your team’s submissions and share reports within your organization
- Use AI to convert PDFs, Excel files, or images into digital forms in seconds—no manual work needed
SOAP Note Template
The SOAP Note is a widely used documentation tool in the healthcare industry, known for its effectiveness in providing clear and organized clinical information.
Standing for Subjective, Objective, Assessment, and Plan, this format allows healthcare professionals to structure patient information in a logical and comprehensive manner.
The SOAP Note facilitates a focused approach to patient care, ensuring that all relevant patient details are captured and considered in the diagnosis and treatment planning process.
This methodical approach is crucial in ensuring continuity of care, especially when multiple healthcare providers are involved.
SOAP Note Template
- Clinic/Hospital Name: ___________
- Patient’s Name: ___________
- Date of Birth: ___________
- Date of Visit: ___________
- Patient ID: ___________
S (Subjective):
- Chief Complaint:
- Reason for the patient’s visit in their own words:
- History of Present Illness:
- Description of the current problem, including symptoms, duration, and severity:
- Past Medical History:
- Previous illnesses, surgeries, chronic conditions, medications:
- Family History:
- Health status or causes of death of immediate family members:
- Social History:
- Lifestyle habits, occupational history, and living conditions:
- Review of Systems:
- General health and functioning of different body systems:
O (Objective):
- Physical Examination:
- Vital signs (e.g., blood pressure, heart rate, respiratory rate):
- Findings from physical examination of different body systems:
- Diagnostic Tests:
- Results from lab tests, imaging studies, or other procedures:
A (Assessment):
- Diagnosis:
- Differential diagnoses and reasoning:
- Analysis of Findings:
- Interpretation of subjective and objective information:
P (Plan):
- Treatment Plan:
- Medications, therapies, lifestyle modifications:
- Referrals to specialists or further testing if needed:
- Follow-Up:
- Schedule for follow-up visits or additional testing:
- Patient Education:
- Information provided to the patient about their condition and treatment:
- Signature:
- Healthcare provider’s signature and credentials:
The SOAP Note Template is a fundamental tool in healthcare for documenting patient encounters in a structured and detailed manner.
This format ensures that all aspects of a patient’s health are thoroughly considered, leading to more accurate diagnoses and effective treatment plans.
It also provides a clear and organized record that is invaluable for continuity of care, especially in settings where multiple healthcare providers are involved.
Regular use of the SOAP Note enhances the quality of patient care and ensures a comprehensive approach to each patient’s health needs.
Choose Connecteam, the #1 Choice for Medical Practices
Revolutionize your medical practice’s daily operations and unleash unparalleled efficiency with Connecteam!
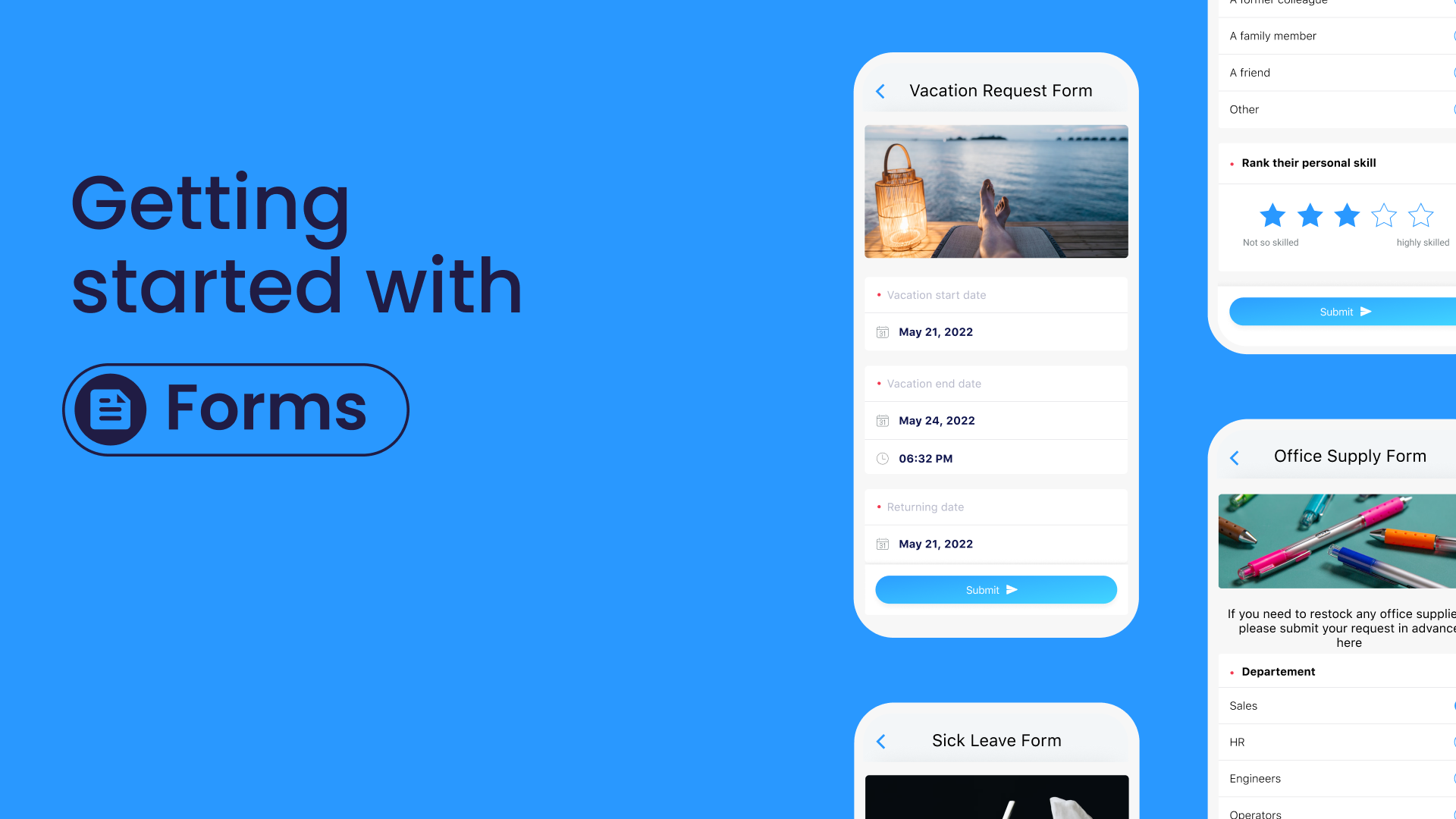
Take charge with our Forms and Checklists feature, effortlessly running your daily tasks and delivering the highest standards. But that’s just the beginning!
Easily create perfect employee schedules with our Employee Scheduler, enabling seamless staff organization and maximizing productivity. Keep a tight grip on employee work times using our Time Clock feature, making precise payroll a breeze and freeing you from mundane administrative tasks.
Stay ahead of the game with Connecteam’s built-in employee Chat, fostering real-time collaboration and empowering your team to deliver extraordinary results.
And don’t forget, continuous growth and skill development are at your fingertips with Connecteam’s comprehensive Training & Onboarding features.
Get started with Connecteam for free today and unlock the true potential of your medical practice’s team!
Watch the video below to see it in action:
Ready to boost your efficiency with our pre-made templates?